Table of Contents
Magnesium is an essential mineral that supports hundreds of biochemical processes, including energy production, protein synthesis, and muscle and nerve function. For those managing diabetes, magnesium’s role in regulating blood glucose levels makes Magnesium for Diabetics a critical consideration. Research highlights its ability to enhance insulin sensitivity and improve glucose metabolism—key factors in diabetes management.
The link between Magnesium for Diabetics and improved health outcomes is well-documented. Insulin resistance, a hallmark of type 2 diabetes, often leads to unstable blood sugar levels. Studies suggest magnesium helps counteract this by optimizing cellular responsiveness to insulin, promoting more efficient glucose uptake. This makes Magnesium for Diabetics a potential ally in reducing hyperglycemia and associated complications.
Magnesium deficiency is alarmingly common among those with diabetes. Factors like poor dietary intake, increased urinary loss due to high blood sugar, and certain medications further deplete magnesium levels. Since low magnesium can worsen insulin resistance and diabetes-related issues, prioritizing Magnesium for Diabetics through diet or supplementation becomes essential.
For individuals with diabetes, addressing magnesium deficiency offers dual benefits: supporting overall wellness and enhancing metabolic health. Foods rich in magnesium—such as leafy greens, nuts, and whole grains—are valuable, but targeted Magnesium for Diabetics supplementation may be necessary to meet daily requirements.
In conclusion, Magnesium for Diabetics is more than a supplement—it’s a strategic tool for improving glucose control and reducing diabetes risks. By understanding its role and ensuring adequate intake, those with diabetes can take proactive steps toward better health. Explore how Magnesium for Diabetics can transform your management plan in the sections ahead.
The Science Behind Magnesium’s Effectiveness

Magnesium plays a critical role in numerous biochemical processes, particularly those related to insulin sensitivity and glucose metabolism. Scientific research indicates that this essential mineral influences the action of insulin, the hormone responsible for regulating blood sugar levels. By enhancing insulin sensitivity, magnesium allows the body to utilize glucose more effectively. This mechanism is vital for individuals with diabetes, as diminished insulin sensitivity often leads to elevated blood sugar levels.
At the cellular level, magnesium acts as a cofactor in over 300 enzymatic reactions. These reactions are crucial for converting glucose into energy, thus facilitating proper cellular function. One of the key enzymes that magnesium activates is phosphofructokinase, which aids in the glycolysis process—where glucose is broken down for energy. Additionally, magnesium contributes to the activation of the enzyme hexokinase, further assisting in sugar metabolism. By ensuring these enzymes function optimally, magnesium supports overall glucose regulation.
Moreover, magnesium interacts with various hormones that are integral to diabetes management. It modulates the secretion of insulin from the pancreas and plays a role in the regulation of glucagon, another hormone that raises blood sugar levels. By maintaining a balanced hormonal environment, magnesium helps in stabilizing blood glucose levels. Furthermore, studies have shown that low magnesium levels can lead to increased inflammation and oxidative stress, both of which are detrimental to metabolic health. As such, a sufficient intake of magnesium may help mitigate these risks, promoting better glycemic control.
Research continues to affirm the vital connection between magnesium and diabetes management. As we delve deeper into its biochemical pathways, we begin to recognize the benefits of maintaining adequate magnesium levels for those living with diabetes. Through its multifaceted roles in cellular processes and hormonal imbalances, magnesium stands out as an essential nutrient in the treatment and prevention of diabetes-related complications.
Magnesium’s Role in Blood Sugar Control
Magnesium is an essential mineral that plays a significant role in various physiological processes in the human body, particularly in individuals with diabetes. It has been increasingly recognized for its contribution to blood sugar regulation and overall glycemic control. Studies have demonstrated a correlation between magnesium levels and blood glucose levels, suggesting that adequate magnesium intake may be beneficial for those managing diabetes.
Research indicates that magnesium assists in the action of insulin, the hormone responsible for regulating blood sugar. When magnesium levels are insufficient, the body may exhibit insulin resistance, making it more challenging to maintain stable blood glucose levels. This resistance is particularly relevant for diabetics, as it can lead to elevated blood sugar levels and further complications related to the disease. Therefore, ensuring an optimal intake of magnesium may enhance insulin sensitivity, a vital factor for effective diabetes management.
Several studies have explored the relationship between dietary magnesium and reduced risk of type 2 diabetes. Findings suggest that higher magnesium intake is associated with improved glycemic control, particularly among those with impaired glucose tolerance. For instance, a systematic review revealed that individuals with higher serum magnesium levels tended to have lower fasting insulin concentrations and better hemoglobin A1c values, indicators of long-term blood glucose levels. Furthermore, supplementation of magnesium has shown promising effects in improving glycemic markers in certain diabetic populations.
In conclusion, the evidence supporting the role of magnesium in blood sugar control highlights its importance in the management of diabetes. Adequate magnesium levels can significantly improve insulin sensitivity and overall glycemic control, making supplementation a potential adjunct therapy for those seeking to optimize their diabetes management strategies.
Sources of Magnesium: Natural and Supplemental
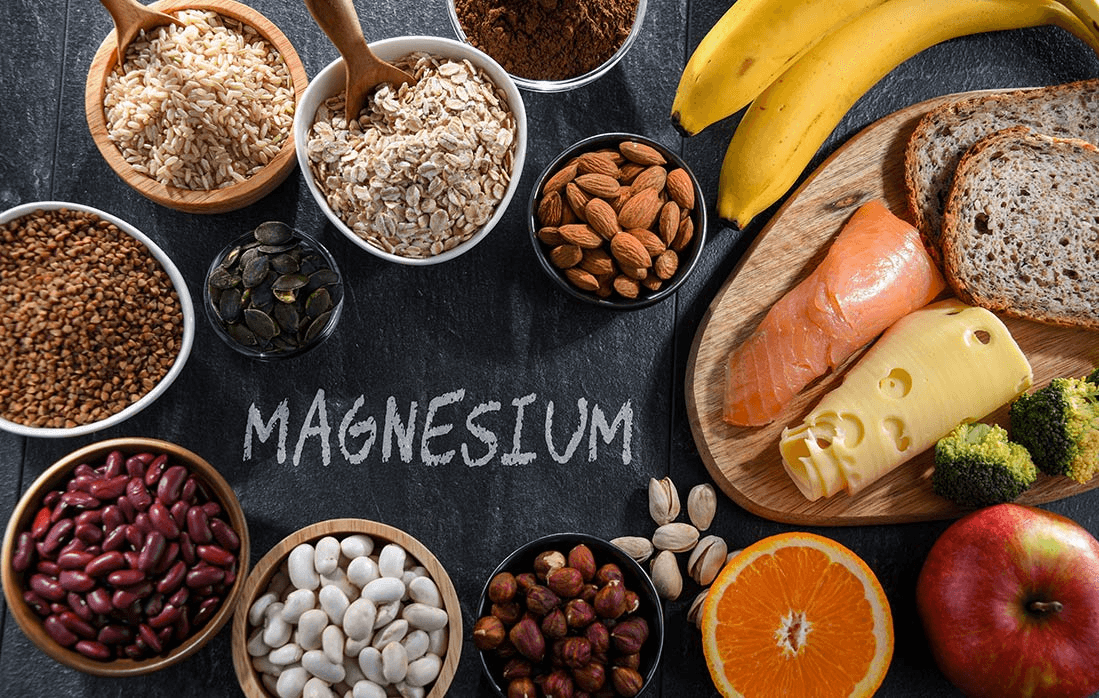
Magnesium is a crucial mineral that plays a significant role in numerous bodily functions, particularly for individuals managing diabetes. Understanding various dietary sources of magnesium can help in ensuring adequate intake. Foods that are rich in magnesium include leafy green vegetables such as spinach and kale, nuts and seeds, legumes, whole grains, and various fruits, particularly bananas and avocados. These foods not only provide magnesium but are also typically high in essential nutrients and fiber, promoting overall health.
Incorporating magnesium-rich foods into daily meals can be simple and enjoyable. For instance, adding spinach to smoothies or salads, snacking on a handful of almonds, or including legumes like lentils in soups and stews can greatly enhance magnesium consumption. Additionally, using whole grains like quinoa and brown rice instead of refined grains can augment not only magnesium intake but also improve glycemic control for diabetics.
While obtaining magnesium from food is ideal, some individuals may require supplementation, particularly if they have difficulty absorbing nutrients or have increased needs. Magnesium supplements come in various forms including magnesium citrate, glycinate, and oxide. Each of these forms has different levels of bioavailability and may affect individuals differently. Therefore, consulting with a healthcare professional before initiating supplementation is recommended.
It is also important to consider potential drawbacks of magnesium supplementation. Overconsumption can lead to gastrointestinal distress or more severe health complications, particularly in those with kidney issues. Therefore, adhering to recommended dosage guidelines is essential to prevent adverse effects while still reaping the benefits of this vital mineral. For most adults, the adequate intake is around 400-420 mg for men and 310-320 mg for women, although these figures can vary based on individual health circumstances.
Potential Risks and Side Effects of Magnesium
While magnesium is an essential mineral that provides numerous benefits, particularly for individuals with diabetes, it is crucial to be aware of the potential risks and side effects associated with its supplementation. Excessive magnesium intake can lead to toxicity, which manifests in various symptoms such as diarrhea, nausea, fatigue, and muscle weakness. Severe cases may result in more serious conditions, including irregular heartbeat and respiratory distress. Therefore, individuals should monitor their magnesium levels and avoid exceeding the recommended dietary allowance.
For those managing diabetes, it’s vital to acknowledge that magnesium can also interact with diabetes medications. For instance, certain oral hypoglycemics may enhance the absorption of magnesium, leading to increased serum levels. Conversely, insulin production and glucose homeostasis can be affected by elevated magnesium levels. This interplay necessitates close monitoring and collaboration with healthcare providers to ensure that magnesium supplementation does not interfere with diabetes management plans.
Furthermore, certain individuals may have existing health conditions, such as renal impairment, where magnesium accumulation could pose a serious threat. Those with compromised kidney function may not be able to excrete excess magnesium effectively, increasing the risk of hypermagnesemia, a condition marked by dangerously high magnesium levels in the blood. For patients with such conditions, magnesium supplementation should be approached with caution.
Before starting any new supplementation regimen, it is essential for individuals with diabetes to consult with healthcare professionals. A thorough evaluation of current medications, health status, and dietary intake can help ensure that the incorporation of magnesium is safe and beneficial. Tailoring magnesium supplementation based on individual needs and circumstances can maximize its advantages while minimizing potential risks.
Magnesium and Diabetic Complications

Magnesium plays a crucial role in various physiological processes, particularly in individuals with diabetes, where it can significantly impact the risk and progression of diabetic complications. Research has shown that magnesium deficiency is common among diabetics and may exacerbate complications such as neuropathy, cardiovascular diseases, and kidney damage.
Neuropathy, characterized by nerve damage often associated with diabetes, can lead to chronic pain and debilitating conditions. Studies indicate that adequate magnesium levels contribute to proper neuronal function, potentially alleviating symptoms and preventing the onset of neuropathy. In one study, higher dietary magnesium intake was linked to a reduced risk of diabetic peripheral neuropathy, underscoring the mineral’s protective role in neurological health for those with diabetes.
Cardiovascular diseases are a significant concern for diabetics, often resulting from poor metabolic control and inflammation. Magnesium is known to have a vasodilatory effect, which may help in reducing blood pressure and improving endothelial function. Epidemiological studies have revealed that higher magnesium levels correlate with a lower incidence of cardiovascular events among individuals with diabetes. These findings suggest that maintaining adequate magnesium levels might play a preventative role in the development of cardiovascular complications.
Kidney damage, or nephropathy, is another major complication in diabetes, often leading to severe health issues. Magnesium has been identified as a protective mineral against kidney damage. Research highlights that magnesium may enhance insulin sensitivity and glucose metabolism, ultimately reducing the burden on the kidneys. Furthermore, some studies suggest that magnesium supplementation can improve renal function among diabetic patients, offering a potential avenue for safeguarding kidney health.
In conclusion, magnesium emerges as a vital mineral in managing diabetic complications. Research continues to affirm its benefits, offering hope for improved long-term health outcomes for diabetics.
Practical Tips for Incorporating Magnesium into Your Diet
Increasing magnesium intake can be seamlessly integrated into daily life with thoughtful meal planning and creative culinary approaches. One of the simplest ways to enhance magnesium levels is by ensuring that meals include magnesium-rich foods. Leafy greens, whole grains, nuts, seeds, and legumes are excellent sources. For instance, incorporating ingredients such as spinach or kale into smoothies or salads can be both nutritious and appealing. A spinach salad topped with sunflower seeds, which are particularly high in magnesium, is an easy and tasty choice.
Whole grains like brown rice or quinoa can serve as hearty bases for meals. Preparing a quinoa salad with black beans, corn, and fresh vegetables not only delivers on flavor but also provides a substantial increase in magnesium. Furthermore, when choosing snacks, opt for nuts and seeds rather than processed options. For example, a handful of almonds, cashews, or pumpkin seeds can serve as a satisfying snack while contributing to daily magnesium goals.
For those looking to add magnesium to their meals without extensive preparation, consider using magnesium-enriched products. There are a variety of foods on the market today, such as magnesium-fortified cereals or energy bars, that can help boost your intake conveniently. Additionally, adding cocoa powder to smoothies or baking recipes can enrich the magnesium content, making it a delightful addition.
Lastly, experimentation in the kitchen can yield delicious results. Trying out various recipes that highlight magnesium-rich foods can be both enjoyable and beneficial. Incorporating new ingredients, such as lentils in soup or using whole grain flour for baking, can introduce vital nutrients into the diet without much effort. By making these adjustments, individuals can enhance their magnesium intake while enjoying a diverse and delicious diet.
Personal Stories: Successes with Magnesium
The journey of managing diabetes can often be fraught with challenges, but for many individuals, the introduction of magnesium into their dietary regimen has led to remarkable improvements in their health. Anecdotes shared by diabetics reveal a pattern of success attributed to increased magnesium intake, underscoring its multifaceted role in diabetes management.
One user, Jane, recounts her experience of living with Type 2 diabetes. Struggling with her blood sugar levels, she decided to explore dietary supplements that could provide her with additional support. After consulting her healthcare provider, Jane began incorporating magnesium-rich foods such as spinach, nuts, and whole grains into her meals. Within a few months, she noticed a significant stabilization in her glucose levels. Jane expressed relief, stating, “Increasing my magnesium intake was a game-changer. I felt more energetic and less reliant on medication to manage my diabetes.”
Similarly, Tom, a recent diabetic diagnosis patient, decided to investigate alternative therapies after finding traditional diabetes management overly challenging. He discovered the potential benefits of magnesium through an online health community. Tom began taking magnesium supplements alongside dietary changes. He reported that his overall health improved, with fewer cravings for sugary snacks and a more stable mood. He remarked, “I always felt like my blood sugar was on a rollercoaster ride. Since adding magnesium, the fluctuations have minimized, and I can focus on living my life rather than just managing diabetes.”
These personal accounts illustrate how integrating magnesium into one’s lifestyle can catalyze significant changes in diabetes management. Each success story not only highlights the correlation between magnesium intake and improved health outcomes but also serves as a source of motivation for others facing similar challenges. The growing awareness of magnesium’s benefits emphasizes the importance of considering this mineral as a valuable component in the diabetic dietary landscape.
Is Magnesium the Magic Bullet for Diabetics?
The discussion surrounding magnesium’s role in diabetes management presents a multifaceted view of its benefits for those living with the condition. As highlighted throughout the article, magnesium serves multiple functions within the body, particularly in regulating blood glucose levels and improving insulin sensitivity. Several studies have indicated that adequate magnesium intake may help reduce the risk of type 2 diabetes and manage existing conditions more effectively, suggesting that this mineral plays a critical role in metabolic processes.
However, it is essential to approach the idea of magnesium as a “magic bullet” with caution. While magnesium supplementation may contribute positively to the overall management of diabetes, it should not be viewed as a standalone solution. Diabetes is a complex condition that requires a comprehensive management plan, which may include dietary changes, physical activity, medication, and regular monitoring of blood glucose levels. Individual responses to magnesium can vary, thus making personalized treatment a key component of effective diabetes care.
Moreover, focusing solely on magnesium neglects other important aspects of holistic health. A balanced diet rich in various nutrients, alongside lifestyle practices such as exercise and stress management, can enhance overall well-being and contribute to better diabetes control. Magnesium can certainly be a valuable part of this larger picture; however, it is one piece of a much more complex puzzle.
Ultimately, while magnesium holds promise in the realm of diabetes management, it should be viewed as part of an integrated approach rather than a magic solution. Patients are encouraged to consult healthcare professionals to develop tailored strategies that suit their individual health needs, emphasizing the importance of a well-rounded and sustainable health plan.











1 Comment