Table of Contents
1. Introduction to Metformin and its Mechanism of Action
Metformin is one of the most commonly prescribed medications for managing type 2 diabetes. It plays a critical role in helping patients maintain optimal blood sugar levels, a crucial aspect of managing diabetes. As a first-line therapy for this condition, metformin is recommended due to its effectiveness, safety profile, and relatively low cost.
The primary way metformin works is by lowering blood glucose levels. It does so through several mechanisms. First, it reduces the liver’s production of glucose, which is a major source of excess blood sugar, especially during fasting. Second, it enhances the body’s sensitivity to insulin, allowing cells to more effectively utilize glucose for energy. This improvement in insulin sensitivity helps to maintain balanced blood sugar levels.
Unlike other diabetes medications, which focus on increasing insulin production by the pancreas, metformin does not directly affect insulin secretion. Instead, it works to correct the underlying issues with insulin resistance and glucose metabolism, which are hallmark features of type 2 diabetes.
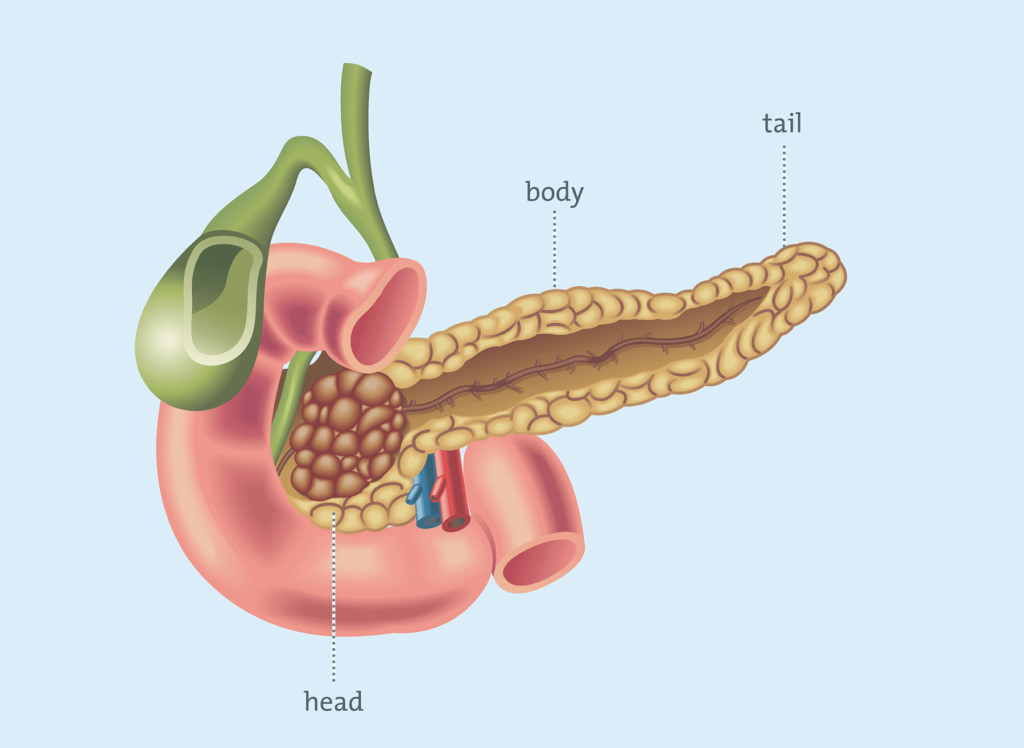
However, many patients with type 2 diabetes may be concerned about the potential effects of metformin on the pancreas, especially since diabetes is intimately linked with pancreatic function. The pancreas plays a crucial role in regulating blood sugar levels by producing insulin. Given that metformin influences the body’s glucose metabolism, some patients may wonder whether it could exert any undue stress on the pancreas.
In this article, we will take a closer look at how metformin interacts with the pancreas, addressing concerns about whether this medication could harm or place strain on this important organ. We will also explore potential risks associated with its use, particularly in individuals with existing pancreatic conditions, and provide recommendations on the safe and effective use of metformin for managing type 2 diabetes. By the end of this discussion, patients and healthcare providers will have a clearer understanding of how metformin works within the body and how to use it safely for optimal diabetes management.
2. Effects of Metformin on the Pancreas
How Metformin Interacts with Pancreatic Cells
While metformin is primarily known for its action on the liver, where it reduces hepatic glucose production, it also has important indirect effects on the pancreas. By lowering blood glucose levels, metformin decreases the demand on pancreatic beta cells, which are responsible for producing insulin. This reduction in workload can be beneficial, as persistent hyperglycemia often leads to beta-cell dysfunction and eventual failure in individuals with type 2 diabetes.
Metformin’s effects on pancreatic cells are not as direct as those of some other diabetes medications. Instead of stimulating insulin secretion, metformin enhances insulin sensitivity in peripheral tissues, such as muscle and fat, allowing cells to use glucose more efficiently. This, in turn, reduces the burden on the pancreas to compensate for insulin resistance, thereby promoting long-term pancreatic health.
Impact on Insulin Production
Unlike sulfonylureas and other insulin secretagogues, which work by stimulating the beta cells to release more insulin, metformin does not directly increase insulin secretion. This distinction is important because excessive insulin production can lead to beta-cell exhaustion over time, potentially worsening diabetes progression. By improving insulin sensitivity and lowering blood glucose levels through other mechanisms, metformin helps maintain a more balanced and sustainable function of the pancreas.
Furthermore, emerging research suggests that metformin may offer protective benefits for pancreatic beta cells. Chronic hyperglycemia, oxidative stress, and inflammation are key factors that contribute to beta-cell dysfunction and destruction in diabetes. Metformin has been found to reduce oxidative stress by enhancing antioxidant enzyme activity and lowering the production of reactive oxygen species (ROS). Additionally, its anti-inflammatory effects may help mitigate beta-cell damage, potentially slowing disease progression.
Potential Long-Term Benefits for Pancreatic Health
The ability of metformin to reduce oxidative stress and inflammation suggests that it may play a role in preserving pancreatic function over time. Some studies indicate that metformin can activate the AMP-activated protein kinase (AMPK) pathway, a crucial regulator of cellular energy homeostasis. Activation of AMPK not only improves insulin sensitivity but may also enhance beta-cell survival by reducing stress-related damage.
While metformin is not a cure for diabetes, its multifaceted effects on glucose metabolism, insulin sensitivity, and pancreatic protection make it one of the most widely prescribed and effective treatments for type 2 diabetes. Ongoing research continues to explore its potential in delaying or even preventing beta-cell failure, offering hope for better long-term management of the disease.
3. Research Studies on Metformin and Pancreatic Health
Key Clinical Studies and Findings
Over the years, extensive research has been conducted to understand the impact of metformin on pancreatic health. Clinical and preclinical studies consistently suggest that metformin is not harmful to the pancreas and may even offer protective effects. Unlike certain diabetes medications that can overstimulate insulin production and contribute to beta-cell exhaustion, metformin works by improving insulin sensitivity and reducing glucose production in the liver, indirectly benefiting the pancreas.
Some studies have explored metformin’s potential in preserving pancreatic beta-cell function, which is crucial for maintaining insulin production in type 2 diabetes patients. Findings suggest that metformin can help mitigate oxidative stress and inflammation—two major contributors to beta-cell deterioration—thereby supporting overall pancreatic health.
Metformin and the Risk of Pancreatitis
Pancreatitis, or inflammation of the pancreas, is a serious condition that can occur in diabetes patients due to various factors, including high blood sugar levels and certain medications. However, research indicates that metformin is not associated with an increased risk of pancreatitis. Unlike some diabetes drugs, such as GLP-1 receptor agonists or DPP-4 inhibitors, which have been linked to a slightly higher risk of pancreatitis, metformin appears to have a neutral or even protective effect.
Several large-scale studies have examined the relationship between metformin use and pancreatitis. Some findings suggest that metformin may lower the risk of pancreatitis compared to sulfonylureas and other glucose-lowering medications. This may be due to metformin’s ability to reduce systemic inflammation and oxidative stress, which are key contributors to pancreatic injury.
Long-term Effects on Pancreatic Function
One of the most significant concerns in type 2 diabetes management is the progressive decline in pancreatic beta-cell function. Research shows that long-term use of metformin does not cause significant damage to the pancreas; rather, it may help slow the deterioration of beta-cell function.
Studies indicate that metformin may promote beta-cell survival by activating the AMP-activated protein kinase (AMPK) pathway, which plays a critical role in cellular energy regulation and stress response. By reducing metabolic stress and improving insulin sensitivity, metformin helps preserve pancreatic function and may delay the progression of type 2 diabetes.
Overall, the evidence suggests that metformin remains a safe and effective medication for diabetes management, with potential benefits for pancreatic health. Ongoing research continues to explore its protective mechanisms, offering hope for improved strategies in preserving beta-cell function and preventing diabetes complications.
4. Potential Risks and Side Effects of Metformin on the Pancreas
Does Metformin Cause Pancreatic Strain?
Metformin is widely regarded as a safe and effective treatment for type 2 diabetes, with no strong evidence suggesting that it directly strains the pancreas. Unlike certain diabetes medications, such as sulfonylureas or incretin-based therapies, metformin does not stimulate the pancreas to produce more insulin. Instead, it primarily works by decreasing glucose production in the liver and enhancing insulin sensitivity in peripheral tissues.
Because metformin does not force the pancreas to work harder, it is less likely to contribute to beta-cell exhaustion, a common concern in diabetes progression. However, some patients experience gastrointestinal side effects, such as nausea, bloating, or diarrhea, which can sometimes be mistaken for pancreatic issues. While these symptoms are typically mild and transient, persistent discomfort should be discussed with a healthcare provider.
Signs of Pancreatic Issues While on Metformin
Although rare, some individuals taking metformin may develop symptoms that could indicate an underlying pancreatic issue. These symptoms include:
- Severe abdominal pain, especially in the upper abdomen or radiating to the back
- Nausea and vomiting, unrelated to usual gastrointestinal side effects
- Unexplained weight loss, which may signal an underlying metabolic or pancreatic condition
If you experience any of these symptoms, particularly persistent or severe abdominal pain, it is crucial to seek medical attention immediately. While metformin itself is not a known cause of pancreatitis, underlying health conditions or interactions with other medications could contribute to pancreatic problems.
Who Is at Risk?
Metformin is generally considered safe for most individuals; however, certain groups may be at a higher risk for pancreatic complications and should use the medication with caution. These include:
- Individuals with a history of pancreatitis: Those who have experienced pancreatitis in the past should consult their doctor before starting metformin, as pre-existing pancreatic inflammation may increase the likelihood of complications.
- Patients with severe gastrointestinal disorders: Chronic digestive conditions, such as gastroparesis or inflammatory bowel disease, may exacerbate gastrointestinal side effects associated with metformin.
- People with significant liver or kidney disease: Since metformin is primarily metabolized by the kidneys, individuals with impaired kidney function should be closely monitored to avoid complications, including the rare risk of lactic acidosis.
Final Considerations
While metformin remains one of the safest and most effective treatments for type 2 diabetes, it is essential for patients to monitor any unusual symptoms and communicate concerns with their healthcare provider. Regular medical check-ups and proper management of diabetes-related complications can help ensure the long-term safety and effectiveness of metformin therapy.
5. Recommendations for Patients Taking Metformin
Monitoring Pancreatic Health
While metformin is generally safe and does not directly harm the pancreas, maintaining overall pancreatic health is essential for individuals managing diabetes. To support pancreatic function and minimize potential risks while taking metformin, consider the following:
- Regular blood tests: Routine monitoring of blood glucose levels, as well as pancreatic enzyme markers such as amylase and lipase, can help detect any early signs of pancreatic stress or dysfunction.
- Following a balanced diet: Eating a diet rich in whole foods, lean proteins, healthy fats, and fiber can help regulate blood sugar levels and reduce strain on the pancreas. Avoiding excessive refined sugars and processed foods may further support pancreatic health.
- Staying hydrated: Proper hydration helps maintain metabolic balance and supports digestive health. Drinking plenty of water can also reduce the risk of gastrointestinal discomfort, a common side effect of metformin.
- Limiting alcohol consumption: Excessive alcohol intake can contribute to both pancreatic inflammation and increased risk of lactic acidosis, a rare but serious complication associated with metformin use. Moderation is key to preventing potential issues.
When to Consult a Doctor
While most people tolerate metformin well, some individuals may experience digestive discomfort or other side effects. It is important to consult a healthcare provider if you experience:
- Persistent stomach pain, especially if it is severe or radiates to the back
- Chronic digestive issues, such as prolonged nausea, vomiting, or diarrhea that does not improve over time
- Unexplained weight loss or appetite changes, which may indicate an underlying condition requiring further evaluation
Your doctor may perform tests, such as blood work or imaging studies, to rule out any pancreatic concerns or assess whether metformin is the right medication for you.
Alternative Diabetes Medications
For patients who cannot tolerate metformin due to side effects or contraindications, alternative diabetes medications may be considered. These include:
- GLP-1 receptor agonists (e.g., Ozempic, Trulicity): These medications help lower blood sugar by mimicking the action of glucagon-like peptide-1 (GLP-1), which stimulates insulin secretion and slows digestion. Some studies suggest they may have additional cardiovascular benefits.
- SGLT2 inhibitors (e.g., Jardiance, Farxiga): These drugs work by preventing glucose reabsorption in the kidneys, leading to lower blood sugar levels and potential weight loss. They may also provide heart and kidney protection.
- DPP-4 inhibitors (e.g., Januvia, Tradjenta): These medications help increase insulin production and decrease glucagon release, though they are generally less effective than GLP-1 receptor agonists.
- Insulin therapy: In cases where oral medications are insufficient, insulin therapy may be necessary to regulate blood sugar levels effectively.
Each diabetes treatment option has its own benefits and potential side effects, so discussing the best approach with a healthcare provider is crucial to achieving optimal diabetes management while minimizing risks.

6. Frequently Asked Questions (FAQs)
1. Can metformin cause pancreatitis?
No, metformin is not known to cause pancreatitis. Unlike certain diabetes medications, such as GLP-1 receptor agonists and DPP-4 inhibitors, which have been linked to a slightly higher risk of pancreatitis, metformin has not shown a direct association with this condition. In fact, some research suggests that metformin may help lower the risk of pancreatitis compared to other diabetes treatments by reducing systemic inflammation and oxidative stress.
2. Does metformin help protect the pancreas?
Yes, some studies indicate that metformin may have protective effects on pancreatic beta cells. By reducing oxidative stress and inflammation—two major contributors to beta-cell dysfunction—metformin may help preserve insulin production and slow the progression of type 2 diabetes. Additionally, its ability to improve insulin sensitivity reduces the workload on pancreatic beta cells, preventing excessive strain.
3. What are the warning signs of pancreatic problems while on metformin?
While pancreatic complications are rare with metformin use, it is important to be aware of potential warning signs that may indicate an underlying issue, such as:
- Severe abdominal pain, especially if it radiates to the back
- Persistent nausea and vomiting, unrelated to common metformin side effects
- Unexplained weight loss, which may signal metabolic or pancreatic dysfunction
If you experience any of these symptoms, seek medical attention promptly to rule out serious conditions like pancreatitis.
4. Can I take metformin if I have a history of pancreatitis?
It depends on your individual medical history. While metformin is generally safe, individuals with a past history of pancreatitis should consult their doctor before taking it. A healthcare provider may evaluate your condition and recommend an alternative treatment if necessary.
5. What other medications should I consider if I cannot take metformin?
If metformin is not suitable for you due to side effects or contraindications, alternative diabetes medications include:
- GLP-1 receptor agonists (e.g., Ozempic, Trulicity) – These medications help lower blood sugar, promote weight loss, and may have additional cardiovascular benefits.
- SGLT2 inhibitors (e.g., Jardiance, Farxiga) – These drugs reduce blood sugar by increasing glucose excretion through the urine and may offer heart and kidney protection.
- DPP-4 inhibitors (e.g., Januvia, Tradjenta) – These medications help regulate blood sugar by enhancing insulin secretion and reducing glucagon production.
- Insulin therapy – In some cases, insulin may be necessary for better blood sugar control.
Your doctor can help determine the best alternative based on your health needs and diabetes management goals.
6. How can I reduce pancreatic stress while taking metformin?
To support pancreatic health while on metformin, consider the following:
- Maintain a healthy diet rich in whole foods, lean proteins, and fiber while avoiding excessive processed sugars and unhealthy fats.
- Stay hydrated to support metabolic function and digestive health.
- Limit alcohol consumption, as excessive drinking can contribute to pancreatic inflammation and other metabolic complications.
- Monitor blood sugar levels regularly to ensure optimal diabetes management and prevent unnecessary stress on the pancreas.
By following these guidelines, you can maximize the benefits of metformin while minimizing potential risks to pancreatic health.
7. Conclusion
Metformin remains one of the most widely used and well-researched medications for managing type 2 diabetes. It effectively lowers blood sugar levels without overstimulating the pancreas, making it a safer option compared to some other diabetes medications. There is no strong evidence to suggest that metformin strains the pancreas; in fact, some studies indicate that it may have protective effects by reducing oxidative stress and inflammation.
However, individuals with a history of pancreatitis or pre-existing pancreatic conditions should consult their doctor before using metformin to ensure it is a suitable choice for them.
By staying informed, monitoring for any unusual symptoms, maintaining a healthy lifestyle, and working closely with healthcare providers, patients can safely use metformin to manage their diabetes while minimizing potential risks. Proper blood sugar management, a balanced diet, and regular medical check-ups are key to ensuring both pancreatic and overall health.











Leave a Comment