Diabetes, a chronic metabolic disorder affecting millions worldwide, arises from the body’s inability to properly regulate blood glucose levels. Accurate and timely diagnosis is crucial for effective management and prevention of long-term complications associated with the disease. This article explores the importance of diagnosing diabetes, outlining the various diagnostic criteria and testing methods employed to identify individuals who may be living with this condition, ultimately highlighting the significance of early detection in improving patient outcomes and overall public health.
Table of Contents
introduction
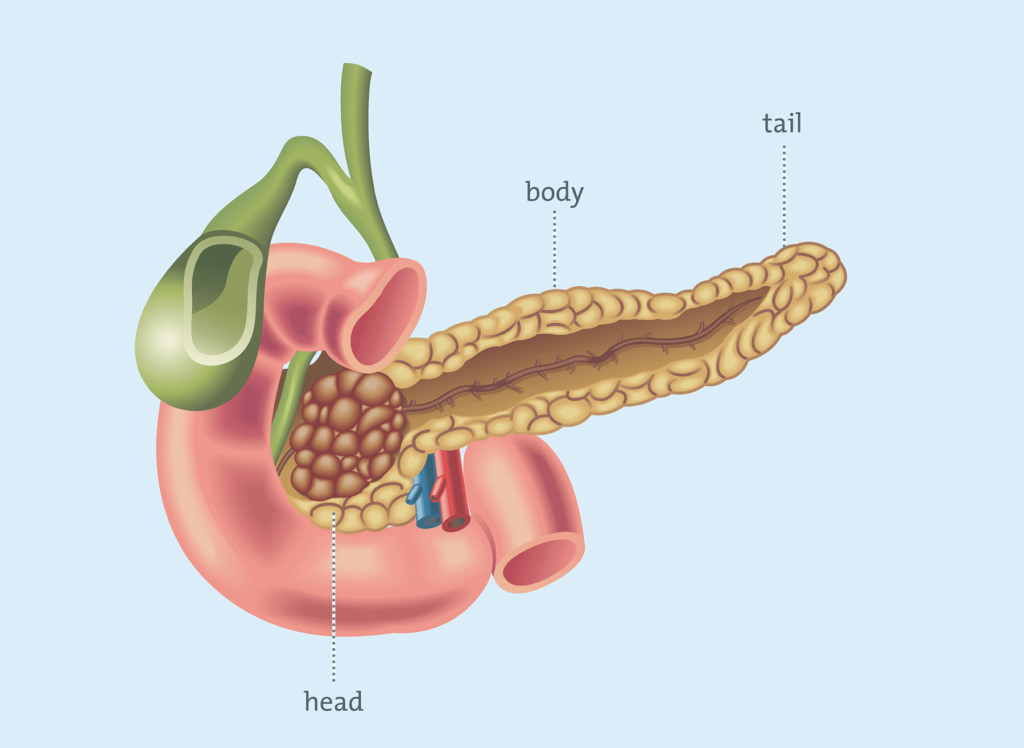
Diabetes is a widespread chronic disease that impacts over 400 million individuals globally, with prevalence continuing to rise due to factors such as aging populations, sedentary lifestyles, and dietary shifts. This metabolic disorder arises when the body fails to produce sufficient insulin—a hormone secreted by the pancreas—or cannot effectively utilize the insulin it produces, leading to impaired regulation of blood glucose levels.
Prolonged elevation of blood sugar, if unmanaged, can result in severe complications, including cardiovascular disease, kidney failure, nerve damage (neuropathy), vision loss, and lower-limb amputations.
Early and precise diagnosis is therefore critical to initiating timely interventions that mitigate these risks and improve long-term health outcomes. Diagnostic methods include the fasting plasma glucose test, which measures blood sugar after an overnight fast; the HbA1c test, reflecting average glucose levels over 2–3 months; and the oral glucose tolerance test, assessing the body’s response to sugar intake. Symptoms such as excessive thirst, frequent urination, unexplained weight loss, and persistent fatigue often prompt these evaluations.
Diabetes is categorized into distinct types: Type 1, an autoimmune condition where the immune system destroys insulin-producing pancreatic cells; Type 2, characterized by insulin resistance and often linked to obesity or genetic factors; gestational diabetes, which emerges during pregnancy; and prediabetes, a reversible precursor marked by elevated blood sugar levels below the diabetes threshold. Treatment strategies emphasize a personalized approach, combining lifestyle modifications like balanced nutrition and regular exercise with pharmacological interventions such as metformin, GLP-1 receptor agonists, or insulin therapy.
Technological advancements, including continuous glucose monitors and insulin pumps, have revolutionized disease management, enabling real-time tracking and precise insulin delivery. Additionally, comprehensive care involves collaboration among endocrinologists, dietitians, and educators to address the multifaceted nature of diabetes, underscoring the importance of patient education and proactive health management to enhance quality of life and reduce complications.
Understanding Diabetes: A Comprehensive Overview
Diabetes is a complex metabolic disorder characterized by chronic hyperglycemia (elevated blood sugar levels) resulting from defects in insulin production, insulin action, or both. Insulin, a hormone synthesized by pancreatic beta cells, acts as a “key” that allows glucose from the bloodstream to enter cells, where it is converted into energy. When insulin function is disrupted—due to insufficient production (as in Type 1 diabetes) or cellular resistance to insulin’s effects (as in Type 2 diabetes)—glucose accumulates in the blood, leading to systemic complications over time. Uncontrolled diabetes can damage blood vessels, nerves, and organs, making early detection and management vital to preventing irreversible harm.
Types of Diabetes
Diabetes is classified into distinct categories, each with unique causes, risk factors, and management approaches:
- Type 1 Diabetes
- Cause: An autoimmune condition where the immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. Genetic predisposition and environmental triggers (e.g., viral infections) may contribute.
- Onset: Typically diagnosed in children, adolescents, or young adults, though it can occur at any age.
- Management: Requires lifelong insulin therapy via injections or pumps, paired with blood sugar monitoring. Recent advancements include hybrid closed-loop insulin delivery systems and research into beta-cell regeneration.
- Type 2 Diabetes
- Cause: Develops due to insulin resistance (cells fail to respond to insulin) coupled with progressive beta-cell dysfunction. Strongly linked to obesity, sedentary lifestyles, genetic factors, and aging.
- Onset: Most common in adults, but rising rates in children correlate with increasing childhood obesity.
- Management: Focuses on lifestyle interventions (diet, exercise, weight loss) and medications like metformin, SGLT2 inhibitors, or GLP-1 receptor agonists. Some individuals may eventually require insulin.
- Gestational Diabetes (GDM)
- Cause: Occurs during pregnancy due to hormonal changes that induce insulin resistance. Risk factors include obesity, advanced maternal age, and a family history of diabetes.
- Implications: Increases the risk of preeclampsia, cesarean delivery, and macrosomia (large birth weight) in infants. Mothers and children have a heightened lifelong risk of developing Type 2 diabetes.
- Management: Controlled through diet, exercise, and sometimes insulin. Blood sugar levels typically normalize post-delivery but require ongoing monitoring.
- Other Types
- Prediabetes: A reversible precursor marked by blood sugar levels above normal but below the diabetes threshold. Lifestyle changes can prevent progression.
- MODY (Maturity-Onset Diabetes of the Young): A rare genetic form caused by single-gene mutations, often misdiagnosed as Type 1 or Type 2.
- LADA (Latent Autoimmune Diabetes in Adults): A slow-progressing autoimmune diabetes with features of both Type 1 and Type 2.
Symptoms of Diabetes
Symptoms arise from the body’s inability to utilize glucose effectively, leading to energy deprivation in cells and glucose buildup in the bloodstream. While manifestations vary by type, common signs include:
- Increased Thirst & Urination: Excess glucose in the blood pulls fluid from tissues, triggering dehydration (polydipsia) and frequent urination (polyuria).
- Unexplained Hunger or Weight Loss: Cells starved of glucose signal hunger (polyphagia), while the body may break down muscle/fat for energy, causing weight loss (common in Type 1).
- Fatigue: Energy deficiency due to impaired glucose uptake.
- Blurred Vision: High blood sugar alters fluid balance in the eyes, temporarily affecting focus.
- Slow-Healing Wounds & Infections: Hyperglycemia weakens immunity and impairs blood flow, delaying healing.
- Numbness/Tingling: Early signs of nerve damage (neuropathy) from prolonged high glucose.
Type-Specific Nuances:
- Type 1: Symptoms often develop abruptly and may include nausea, vomiting, or diabetic ketoacidosis (DKA), a life-threatening condition.
- Type 2: Symptoms may be subtle or absent for years, leading to delayed diagnosis.
Diagnosing Diabetes
Accurate diagnosis relies on standardized tests interpreted alongside clinical symptoms:
- Fasting Plasma Glucose (FPG) Test
- Procedure: Measures blood sugar after an 8-hour fast.
- Diagnostic Threshold: ≥126 mg/dL (7.0 mmol/L) on two separate tests.
- Oral Glucose Tolerance Test (OGTT)
- Procedure: Assesses blood sugar before and 2 hours after consuming a 75g glucose drink.
- Diagnostic Threshold: ≥200 mg/dL (11.1 mmol/L) at 2 hours. Often used for gestational diabetes screening.
- Hemoglobin A1C Test
- Procedure: Reflects average blood glucose over 2–3 months by measuring glycated hemoglobin.
- Diagnostic Threshold: ≥6.5%. Advantages include no fasting requirement, though results may be skewed by conditions like anemia.
- Random Plasma Glucose Test
- Procedure: Blood sugar measured at any time, regardless of meal timing.
- Diagnostic Threshold: ≥200 mg/dL (11.1 mmol/L) with classic symptoms (e.g., thirst, urination).
Additional Considerations:
- Gestational Diabetes Screening: Conducted between 24–28 weeks of pregnancy using a 1-hour (non-fasting) or 3-hour OGTT.
- Confirmatory Testing: A single abnormal test with symptoms suffices for diagnosis; asymptomatic cases require two abnormal results.
Tables:
| Test | Description | Result Indicating Diabetes |
|---|---|---|
| Fasting Plasma Glucose Test | Measures blood sugar level after an overnight fast | 126 mg/dL or higher |
| Oral Glucose Tolerance Test | Measures blood sugar level before and after drinking a sugary drink | 200 mg/dL or higher two hours after drinking the drink |
| Hemoglobin A1C Test | Measures average blood sugar level over the past three months | 6.5% or higher |
Read More: What Is Type 2 Diabetes? Causes, Symptoms And Treatment – Diavetes
Why Early Detection is Key
Diabetes often begins its insidious journey long before symptoms become noticeable. This silent progression, where elevated blood sugar levels gradually damage vital organs, underscores the critical importance of early detection. For many, especially those in high-risk groups, proactive screening isn’t just recommended – it’s a vital step towards safeguarding long-term health and preventing irreversible complications.
The danger of undiagnosed diabetes lies in its very nature – it’s a stealthy saboteur. Elevated blood glucose, if left unchecked over years, can silently attack the delicate networks of blood vessels throughout the body. This damage can lead to a cascade of serious health issues, including heart disease, stroke, kidney failure, nerve damage (neuropathy), and vision loss (retinopathy). Imagine a slow leak in a pipe – initially unnoticed, it eventually causes significant structural damage. Undiagnosed diabetes operates similarly, silently eroding health from within.
Recognizing who is most vulnerable is the first step towards proactive detection. Individuals carrying extra weight, those with a family history of diabetes, and those with pre-existing cardiovascular disease fall squarely into high-risk categories. Factors like age, ethnicity, and sedentary lifestyles also contribute to increased risk. For these individuals, regular screening becomes paramount. Simple and readily available blood glucose tests, including fasting plasma glucose and HbA1c tests, can provide crucial insights into blood sugar levels and identify potential pre-diabetes or diabetes.
Fortunately, the landscape of diabetes diagnostics is constantly evolving. Advances in technology are providing clinicians with increasingly sophisticated tools to detect and classify diabetes with greater precision. Continuous Glucose Monitors (CGMs), once primarily used by individuals already diagnosed with diabetes, are now finding applications in screening and early diagnosis. These wearable devices provide real-time glucose readings, offering a far more comprehensive picture of glucose fluctuations than traditional single-point-in-time tests.
Furthermore, genetic testing is playing a growing role, particularly in identifying monogenic diabetes – forms of diabetes caused by single gene mutations. Understanding the genetic basis of diabetes allows for more precise classification and tailored treatment strategies, moving away from a one-size-fits-all approach. These advancements are not just about diagnosing diabetes; they are about understanding the nuances of the condition in each individual, paving the way for more effective and personalized interventions.
The true power of early detection lies in the opportunity for early intervention. Prompt diagnosis allows individuals to work with healthcare professionals to manage blood sugar levels effectively, often through lifestyle modifications like diet and exercise, and, when necessary, medication. This proactive approach not only stabilizes blood sugar but also significantly reduces the risk of developing debilitating and life-threatening complications. By acting early, we can prevent the “slow leak” from turning into a catastrophic flood of health problems.
Ultimately, early detection of diabetes is not just about identifying a disease; it’s about empowering individuals to take control of their health trajectory. It reinforces the powerful adage: knowledge is power – and prevention. Knowing your risk factors, understanding the importance of screening, and embracing the advancements in diagnostic tools are crucial steps in safeguarding your future well-being. Don’t let the silent threat of undiagnosed diabetes compromise your health. Take the first step today – talk to your doctor about diabetes screening, and embrace the power of early detection for a healthier tomorrow.
Treatment Options for Diabetes
The treatment options for diabetes vary depending on the type, severity, and individual health condition of the patient. The primary objective of diabetes management is to regulate blood sugar levels effectively and prevent long-term complications such as nerve damage, kidney disease, heart disease, and vision problems.
Type 1 Diabetes
Type 1 diabetes is an autoimmune condition in which the body’s immune system mistakenly attacks insulin-producing cells in the pancreas. As a result, the body is unable to produce insulin, making insulin therapy essential for survival. Treatment typically involves:
- Insulin Therapy: Insulin must be administered through multiple daily injections or an insulin pump to regulate blood sugar levels. Various types of insulin exist, including rapid-acting, short-acting, intermediate-acting, and long-acting insulin, depending on the patient’s needs.
- Blood Sugar Monitoring: Patients with type 1 diabetes need to check their blood sugar levels multiple times a day using a glucose meter or continuous glucose monitoring (CGM) systems.
- Diet and Lifestyle Management: Although insulin therapy is essential, maintaining a balanced diet, counting carbohydrates, and exercising regularly play a crucial role in stabilizing blood sugar levels and improving overall health.
Type 2 Diabetes
Type 2 diabetes is the most common form of diabetes, primarily associated with insulin resistance, where the body does not use insulin effectively. The treatment approach varies based on the severity of the condition and may include:
- Lifestyle Modifications: The first line of treatment often includes changes in diet, regular physical activity, and weight management. A well-balanced diet that includes whole grains, lean proteins, healthy fats, and fiber can help regulate blood sugar levels. Exercise, such as walking, jogging, or strength training, improves insulin sensitivity.
- Oral Medications: If lifestyle modifications are insufficient, doctors may prescribe oral medications like metformin, which helps lower blood sugar levels by reducing glucose production in the liver and improving insulin sensitivity. Other medications, such as sulfonylureas, SGLT2 inhibitors, and DPP-4 inhibitors, may also be prescribed depending on individual needs.
- Injectable Medications: In some cases, injectable drugs like GLP-1 receptor agonists or even insulin may be required if blood sugar levels remain uncontrolled.
Gestational Diabetes
Gestational diabetes develops during pregnancy and usually resolves after childbirth. However, proper management is crucial to prevent complications for both the mother and baby. Treatment strategies include:
- Dietary Adjustments: Eating balanced meals with a focus on whole foods, fiber-rich carbohydrates, and lean proteins can help regulate blood sugar levels.
- Regular Physical Activity: Engaging in moderate exercise, such as walking or prenatal yoga, can improve insulin sensitivity and help manage blood sugar.
- Blood Sugar Monitoring: Pregnant women with gestational diabetes must monitor their blood sugar levels frequently to ensure they remain within a healthy range.
- Medication: If lifestyle changes are not sufficient, insulin therapy or oral medications like metformin may be prescribed under medical supervision.
Managing diabetes requires a personalized approach based on the specific type and individual health needs. While lifestyle modifications form the foundation of diabetes treatment, medical interventions such as insulin therapy and medications may be necessary to achieve optimal blood sugar control. Regular monitoring, adherence to prescribed treatments, and collaboration with healthcare providers can help prevent complications and improve the overall quality of life for individuals living with diabetes.
Frequently Asked Questions (FAQs) About Diabetes
Can diabetes be cured?
No, diabetes is a chronic condition that currently has no cure. However, it can be effectively managed through a combination of lifestyle modifications, medication, and, in some cases, medical procedures. People with type 1 diabetes require lifelong insulin therapy, while those with type 2 diabetes can sometimes achieve remission through significant weight loss, healthy eating, and regular physical activity. Although diabetes cannot be permanently eliminated, proper management can prevent complications and improve quality of life.
How often should I check my blood sugar level?
The frequency of blood sugar monitoring depends on the type of diabetes, individual health status, and the treatment plan prescribed by your healthcare provider:
- Type 1 Diabetes: Blood sugar should be checked multiple times daily, including before meals, before and after exercise, and at bedtime. Continuous glucose monitoring (CGM) systems can provide real-time data and alerts for better control.
- Type 2 Diabetes: Those managing diabetes through lifestyle changes may not need to check as frequently, but individuals taking medications or insulin may need to test their levels once or several times a day, as advised by their doctor.
- Gestational Diabetes: Pregnant women with gestational diabetes often need to check their blood sugar levels multiple times a day, particularly before and after meals, to ensure levels remain within the target range.
Your healthcare provider will recommend a personalized monitoring schedule based on your condition.
What are the complications of diabetes?
If left unmanaged, diabetes can lead to serious health complications, including:
- Cardiovascular Disease: High blood sugar levels increase the risk of heart disease, high blood pressure, stroke, and poor circulation, which can lead to complications such as heart attacks.
- Nerve Damage (Neuropathy): Prolonged high blood sugar can damage nerves, causing numbness, tingling, or pain, especially in the hands and feet. Severe cases can lead to foot ulcers and amputations.
- Kidney Damage (Nephropathy): Diabetes can harm kidney function, potentially leading to kidney failure and the need for dialysis or a transplant.
- Eye Problems (Retinopathy): Uncontrolled diabetes can cause vision problems, including diabetic retinopathy, cataracts, and glaucoma, which may lead to blindness if untreated.
- Foot Complications: Poor circulation and nerve damage increase the risk of infections and slow wound healing, which may require amputation in severe cases.
- Skin and Oral Health Issues: People with diabetes are more prone to skin infections, gum disease, and slow wound healing.
- Mental Health Impact: Living with diabetes can contribute to stress, anxiety, and depression, making emotional and psychological support an important aspect of diabetes care.
Proper diabetes management, including regular check-ups, a balanced diet, physical activity, and adherence to medication, can significantly reduce the risk of these complications.
“Take care of your body. It’s the only place you have to live.” – Jim Rohn
Conclusion
Diabetes is a chronic and serious condition that affects millions of people worldwide, with its prevalence steadily increasing. Early detection and accurate diagnosis are essential in managing the disease effectively and preventing long-term complications such as heart disease, kidney failure, nerve damage, and vision problems.
Recognizing the early signs of diabetes—such as frequent urination, excessive thirst, unexplained weight loss, fatigue, and blurred vision—can help individuals seek medical attention promptly. If you experience any of these symptoms, it is crucial to consult a healthcare provider for proper evaluation, blood sugar testing, and diagnosis. Early intervention, including lifestyle modifications and, if necessary, medication, can help control blood sugar levels, reduce the risk of complications, and improve overall health and quality of life.
Taking proactive steps toward diabetes management can make a significant difference. Regular check-ups, a healthy diet, physical activity, and adherence to prescribed treatments can help individuals with diabetes lead healthier, more fulfilling lives.
References
- American Diabetes Association. (2021). Diabetes Diagnosis. https://www.diabetes.org/about-diabetes//diagnosis
- Mayo Clinic. (2021). Diabetes. https://www.mayoclinic.org/diseases-conditions/diabetes/symptoms-causes/syc-20371444
- National Institute of Diabetes and Digestive and Kidney Diseases. (2021). Diabetes Tests & Diagnosis. https://www.niddk.nih.gov/health-information/diabetes/overview/tests-diagnosis
Note: This article is intended to provide general information about diagnosing diabetes and should not be used as a substitute for medical advice from a healthcare provider. If you experience any symptoms of diabetes, it is essential to consult a healthcare provider for proper diagnosis and treatment.